“Teen stomach pain ignored” sounds like the kind of phrase that belongs in a distant headline—something clinical, abstract, easy to scroll past between news updates and lifestyle tips. I used to think that way too.
Until those words became deeply personal, attached to my own home, my own child, and a slow-moving crisis that unfolded right in front of me.
Those three weeks rewired how I understand health, parental instincts, and the real cost of delayed medical care. They taught me how easily symptoms can be minimized, how denial can feel comforting, and how quickly a situation can escalate when warning signs are explained away instead of investigated.
My name is Melissa Grant. I live with my husband, Derek, and our daughter, Hannah, in a quiet suburb outside Denver. It’s the kind of place associated with good schools, safe streets, and the unspoken belief that serious illness happens somewhere else—usually to other people.
That assumption nearly cost us everything.
The First Complaint That Seemed So Ordinary
The first time Hannah mentioned her stomach pain, it felt almost routine. She stood in the kitchen doorway after school, backpack hanging from one shoulder, her posture slightly slumped in a way I initially chalked up to teenage fatigue.
Her face, though, caught my attention. She looked pale—not dramatically so, but enough that something felt off.
“Mom… my stomach’s been hurting all day,” she said, one hand resting protectively on her lower abdomen.
I turned from the stove and touched her forehead. She wasn’t feverish. She wasn’t crying. She wasn’t asking to stay home from school or seeking sympathy.
“Probably something from the cafeteria,” I said gently. “Sit down. I’ll make you some tea.”
That explanation fit neatly into the mental box we all keep labeled normal teenage issues. Minor digestive trouble. Stress. A stomach bug. Nothing that required immediate health insurance claims, specialist visits, or complicated decisions.
That night, Hannah barely ate dinner. She pushed food around her plate, excused herself early, and went to bed without complaint. Derek noticed but waved it off.
“She’s just not hungry,” he said. “Teenagers are weird about food.”
I wanted to believe him. Belief made things simpler.
When Pain Doesn’t Fade—It Persists
But the pain didn’t go away.
By the end of the first week, Hannah mentioned it every day. Not dramatically. Not urgently. Just consistently. She still went to school. She still did her homework. She still tried to keep up with her routine.
But I began noticing subtle changes that didn’t sit right.
She walked more slowly, like her body resisted movement. She skipped meals without making a fuss. She slept earlier but woke up looking exhausted. Dark circles settled under her eyes despite getting what should have been enough rest.
I mentioned it to Derek again.
“She’s stressed,” he said, barely looking up from his laptop. “Exams, friends, hormones. You remember being sixteen. Everything feels worse than it is.”
“But she’s losing weight,” I said. “Her jeans don’t fit anymore.”
“Growth spurt,” he replied confidently. “Or she’s skipping lunch. Don’t turn this into something bigger than it is.”
His certainty made me second-guess myself. I hated how effective it was. I started wondering if I was projecting anxiety, if I was overreacting the way parents sometimes do.
This is where early intervention quietly slipped through our fingers.
The Second Week: Symptoms That Couldn’t Be Explained Away
During the second week, everything escalated.
Hannah began waking up at night to vomit. At first, it happened every few days. Then every night. I sat with her on the cold bathroom floor, holding her hair back as her body shook.
“It feels like something’s squeezing inside,” she whispered one night. “Like it’s twisting.”
That word—twisting—lodged itself in my chest and refused to leave.
Vomiting, abdominal pain, weight loss, fatigue—these are not trivial symptoms. In hindsight, they are textbook red flags that often warrant imaging, bloodwork, and immediate medical evaluation.
At the time, though, doubt still hovered.
The next morning, I told Derek we needed to see a doctor.
“This isn’t normal,” I said. “She’s getting worse.”
He sighed, clearly irritated.
“They’ll say it’s a virus or anxiety and send us home with a bill,” he said. “You’re feeding into it.”
I tried to explain what I was seeing. The pain. The weakness. The nightly vomiting. But the conversation ended the same way it always did—him calm, and me feeling unreasonable.
Meanwhile, Hannah continued to fade.
Watching a Child Grow Weaker Is Its Own Kind of Trauma
By the third week, fear replaced doubt entirely.
Hannah could barely eat toast. She leaned against walls when she walked. She no longer laughed. Her energy was gone, replaced by a bone-deep exhaustion that made her look older than sixteen.
One evening, I found her sitting on her bed still dressed, backpack on the floor, tears sliding silently down her face. She wasn’t crying loudly because she didn’t want to scare me.
That restraint broke my heart.
The next morning, I woke to find her drenched in sweat, sheets tangled around her legs. Her skin felt clammy under my hand.
“Mom,” she whispered, eyes barely open, “it really hurts.”
That was the moment something inside me snapped into clarity.
I didn’t call Derek. I didn’t debate. I didn’t rationalize.
I grabbed my keys.
“We’re going to the hospital. Now.”
The Emergency Room Where Everything Changed
The emergency room was blindingly bright, the kind of sterile light that strips away denial. Hannah leaned heavily against me as we checked in. Her weight felt wrong—lighter than it should be, yet strangely difficult to support.
One look from the triage nurse and we were taken back immediately. That urgency terrified me more than waiting ever could have.
Everything happened fast. Blood tests. IV fluids. Questions Hannah was too exhausted to answer, so I answered for her. When the doctor pressed on her abdomen and she cried out, it felt like the pain hit me directly.
Machines hummed. Curtains shifted. Time lost its shape.
Derek texted once: How’s it going?
I couldn’t respond.
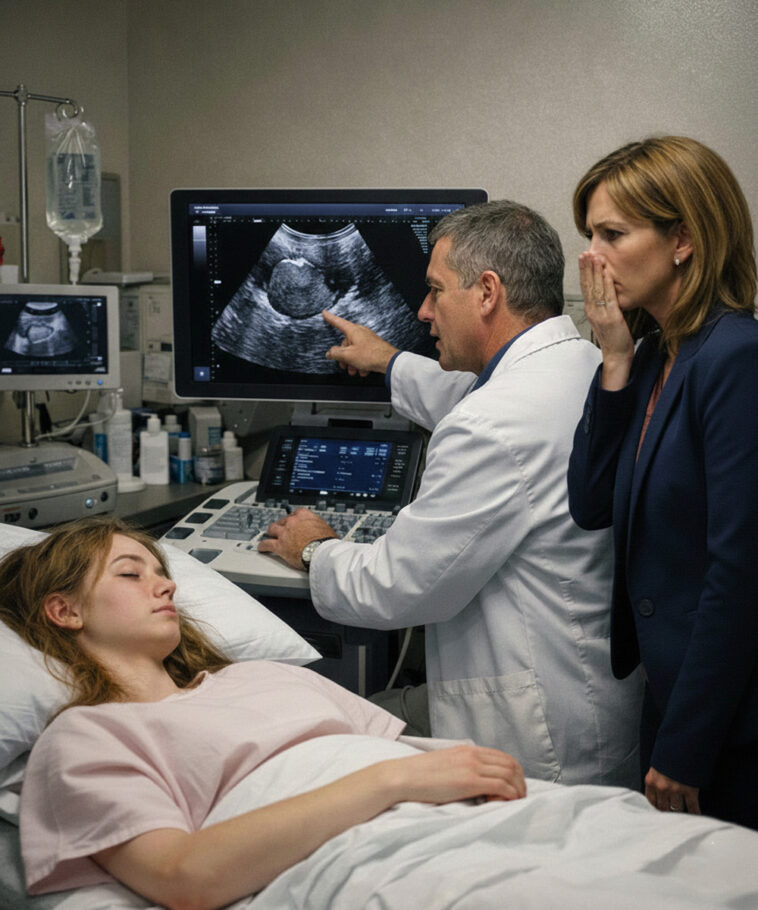
A young doctor with calm eyes introduced himself as Dr. Lawson.
“We’ve done an ultrasound,” he said. “We’re ordering a CT scan for a clearer picture.”
“What are you looking for?” I asked.
“Anything that explains the pain and vomiting,” he replied carefully.
That careful tone mattered.
The Scan That Made My Legs Give Out
When Hannah was wheeled away for imaging, I sat alone, staring at the empty bed. Guilt flooded me—every moment I’d hesitated, every time I’d chosen peace over insistence.
Dr. Lawson returned with an older physician. They pulled the curtain closed.
I knew before they spoke.
“Mrs. Grant,” the older doctor said gently, “your daughter has a large mass in her abdomen.”
The word mass didn’t register.
“It appears to be a tumor,” he continued. “It’s pressing against her organs. We need to admit her and prepare for surgery.”
My vision dimmed. The room tilted. I reached for the bed rail, but my legs gave out anyway.
In that moment, medical terminology stopped being abstract. It became immediate, terrifying, and real.
Surgery, Waiting Rooms, and the Cost of Delay
Everything after that happened in sharp bursts. Consent forms. Explanations. Surgical plans. Derek arrived, pale and shaken when I said the word tumor. For the first time, he didn’t argue. He just sat down and buried his face in his hands.
Hannah went into surgery that evening. As they wheeled her away, she smiled at me.
“Love you, Mom,” she said—like she was the one comforting me.
The waiting room stretched endlessly. Every opening door sent my heart racing. I replayed every dismissed symptom, every internal debate, every moment I’d doubted my own instincts.
When the surgeon finally emerged, mask hanging loose, exhaustion etched into his face, I could barely breathe.
“We removed the tumor,” he said. “It was large, but we got it all. Now we wait for pathology.”
When Relief Feels Almost Painful
Days later, the results came back.
Benign.
The word hit me with a force I wasn’t prepared for. I collapsed in the hallway, sobbing with relief so intense it hurt. Derek held me, whispering apologies through his own tears.
We were lucky. In a way that feels uncomfortable to say out loud, we were incredibly lucky.
Not every story ends this way. Not every delay is survivable. Not every family gets a second chance.
What This Experience Taught Me About Health and Advocacy
“Teen stomach pain ignored” nearly cost my daughter everything—not because we didn’t love her, but because doubt is persuasive and denial is comfortable.
This experience taught me that:
-
Persistent pain is never “just attention”
-
Weight loss and vomiting warrant immediate medical assessment
-
Parents must sometimes override reassurance—even from partners
-
Early imaging and diagnostics can save lives
-
Listening is a form of protection
Now, when Hannah says something hurts, I listen. Immediately. Without debate. Without dismissal.
Because sometimes, a mother’s fear is the only alarm bell a child has.
And sometimes, trusting that instinct is the most important decision you’ll ever make.
As you were.