My husband insisted our fifteen-year-old daughter was pretending. “She’s exaggerating. Don’t waste time or money on doctors,” he said—flat, dismissive, final.
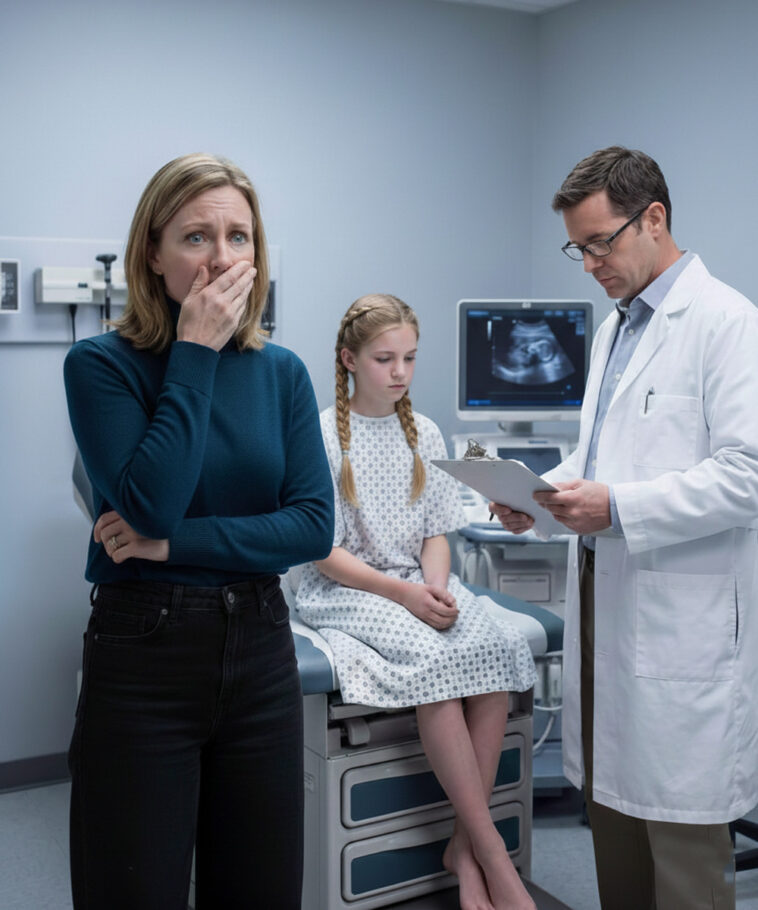
But I trusted my instincts. I took her to the hospital without telling him. And when the doctor studied the scan, lowered his voice, and said, “There’s something inside her,” my world collapsed.
I screamed because there was nothing else left to do.
This is a story about parental intuition, teen health, and the devastating cost of not listening—told plainly, carefully, and with respect for what no child should ever endure.
The Signs We’re Told to Ignore
Long before the hospital, I knew something was wrong.
For weeks, my daughter Hailey complained of persistent nausea, sharp stomach pain, dizziness, and exhaustion that didn’t match the energetic girl she used to be. Soccer practices were skipped. Her camera gathered dust. Laughter disappeared. She kept her hood up indoors and flinched whenever someone asked how she felt.
My husband, Mark, brushed it off. “She’s faking. Teenagers love drama,” he said. “Doctors are a waste of time and money.”
I watched anyway.
Hailey ate less and slept more. She winced tying her shoes. Her weight dropped, her color faded, and the spark in her eyes went out. It felt like watching a child vanish behind frosted glass—present, but unreachable.
From a healthcare standpoint, these were red flags. Persistent abdominal pain in adolescents can signal many things—gastrointestinal issues, hormonal imbalances, infection, stress-related illness, and more. What matters is not guessing. What matters is checking.
The Night Everything Became Clear
One night, after Mark went to bed, I found Hailey curled on her mattress, clutching her stomach. Her skin was pale; her pillow soaked with tears.
“Mom,” she whispered, “it hurts. Please make it stop.”
That was the moment every doubt vanished.
The next day, while Mark was at work, I drove her to St. Helena Medical Center. She stared out the window in silence. The nurse checked vitals. Blood tests were ordered. An ultrasound followed. I sat wringing my hands until they trembled.
When Dr. Adler returned, his expression carried weight.
“Mrs. Carter,” he said gently, “we need to talk.”
Hailey sat shaking beside me.
Lowering his voice, the doctor said, “The scan shows there is something inside her.”
I stopped breathing.
A Diagnosis No Parent Expects
“Inside her?” I echoed. “What does that mean?”
He hesitated—and that pause said everything.
“We need to discuss this privately,” he said. “Please prepare yourself.”
The room felt smaller. The air thick. Before reality could settle, I screamed.
Then came the words no parent is ready to hear: Hailey was pregnant—about 12 weeks.
Silence swallowed the room.
“That’s impossible,” I whispered. “She’s fifteen.”
Hailey sobbed, folding into herself. I reached for her. She didn’t pull away from me—only from the truth.
From a medical and legal perspective, the next steps were immediate. Because of her age, a social worker was required. Procedures were explained. Options were discussed. My ears rang as if underwater.
When Healthcare and Child Protection Intersect
A social worker named Lauren arrived and asked to speak with Hailey alone. I paced the hallway, nails digging into my palms as minutes stretched.
When Lauren returned, her expression was heavy.
“Mrs. Carter,” she said softly, “we need to talk.”
Hailey’s pregnancy was not consensual. Someone had hurt her. This was not her choice.
My head spun.
Lauren asked a question that struck like a slap: “Does Hailey feel safe at home?”
I said yes—but the word felt brittle.
“Sometimes children stay silent,” Lauren said gently, “to protect the people who are supposed to love them.”
Suddenly, memories rearranged themselves: Hailey shrinking when Mark entered a room. Her dread of weekends. Her fear of being left alone.
From a child advocacy standpoint, these patterns matter. Silence is not consent. Fear often looks like obedience.
Lauren recommended we stay somewhere else that night. I agreed. We went to my sister’s house.
The Truth No One Wants to Face
At dawn, we met police officers at a child advocacy center designed to feel safe—soft lighting, stuffed animals, calm voices. Hailey gave her statement with care and support.
Afterward, Detective Morris approached me.
“She told us who it was,” he said quietly.
My breath stopped.
“It was Mark.”
The world shattered.
My husband. The man who dismissed her pain. The man who told me doctors were a waste.
From a legal perspective, things moved quickly. A warrant was issued. Mark was arrested. When we heard “He’s in custody. Your daughter is safe,” I finally breathed.
Picking Up the Pieces
In the weeks that followed, I filed for divorce. Hailey began trauma-informed therapy. Charges were filed. Healing was slow.
We moved into a small apartment across town. It wasn’t perfect, but it was safe.
From a mental health standpoint, recovery takes time. From a family law standpoint, protection orders and custody arrangements mattered. From an insurance standpoint, therapy coverage and medical care became priorities.
Hailey joined a support group. Slowly, she reclaimed pieces of herself—art, laughter, her voice.
One night, eating takeout on our couch, she said, “Thank you for believing me, Mom.”
I squeezed her hand. “I always will.”
Why This Story Matters
This story isn’t about blame—it’s about listening.
If a teen reports pain, believe them. If symptoms persist, seek medical care. If something feels wrong, trust your instincts. Healthcare decisions aren’t just clinical—they’re moral.
Ignoring symptoms doesn’t save money. It delays answers. It risks lives.
And sometimes, listening changes everything.
Just that.