During my two-week stay in the hospital, silence became my closest companion. The kind of silence that isn’t peaceful, but persistent. The kind that presses in gently at first and then settles deep into your chest when the hours stretch too long and the nights refuse to end. My children lived in different cities, several hours away by car, each with lives full of work, family obligations, and responsibilities that no longer belonged to me. My friends checked in when they could, their voices kind but hurried, their concern genuine yet distant. Visiting hours came and went, often without a single familiar face crossing the threshold of my room. Each day unfolded slowly, marked not by conversation or laughter, but by the soft beeping of monitors, the rustle of curtains, and the careful footsteps of nurses changing shifts. Hospitals have their own rhythm, and when you’re alone inside it, time feels heavier than it does anywhere else.
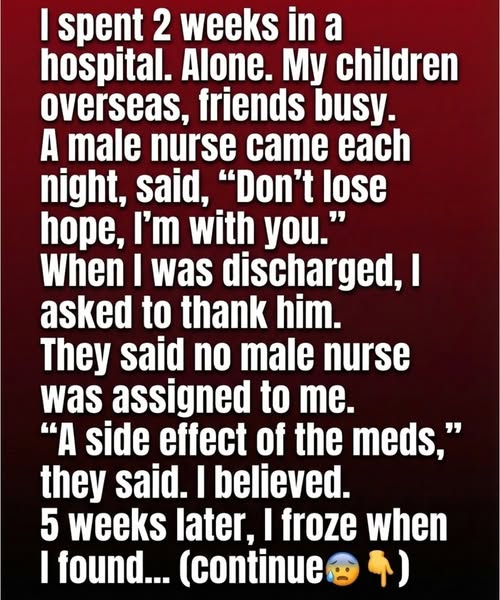
The Weight of Loneliness During Recovery
I tried to stay optimistic. I told myself that this was temporary, that healing takes patience, and that my body needed rest more than distraction. Doctors spoke in reassuring tones about progress, lab results, and treatment plans. They explained things carefully, using words tied to health outcomes, recovery timelines, and medical indicators meant to inspire confidence. On paper, everything looked manageable. But loneliness doesn’t show up on charts. It doesn’t appear in insurance paperwork or discharge summaries. It arrives quietly, usually after the lights dim, when the hallway noise fades and you’re left alone with your thoughts. It doesn’t announce itself dramatically. It simply sits beside you, heavy and persistent, making even the strongest moments feel fragile. At night, when pain medication softened the edges of discomfort but sharpened awareness, I felt the absence of voices more clearly than anything else. Healing the body is one thing. Sitting with the silence while you do it is another entirely.
The One Constant in the Long Evenings
Every night, though, there was one constant that anchored me. Just before the ward settled into complete stillness, a nurse would come by. He moved quietly, never rushed, as if he understood that the evening carried a different weight than the day. He asked how I was feeling, not in the automated way you expect from busy hospital staff, but with genuine attention. He adjusted my blanket, checked the monitors, made sure the IV line was comfortable, and spoke a few words before leaving. “Rest now.” “Don’t give up.” “You’re doing better than you think.” They were simple phrases, the kind you might overlook anywhere else. But in that sterile room, surrounded by medical equipment and unfamiliar smells, those words mattered more than I can explain. They made me feel seen, not as a patient number tied to billing codes and insurance approvals, but as a person navigating one of the most vulnerable chapters of life.
Feeling Seen Beyond the Medical Chart
In those moments, I felt noticed in a way that went beyond clinical care. Hospitals are designed to keep you alive, to monitor vitals, to manage risk and liability, and to document every intervention for legal and financial accountability. But what often gets lost is the human experience unfolding inside those walls. His presence became part of my routine, something I quietly looked forward to each night. It was a reassurance that I wasn’t completely alone, even if my family and friends couldn’t be there. He never lingered too long. He never crossed any boundaries. He simply showed up consistently, and consistency, I learned, can feel like hope when everything else feels uncertain.
Discharge Day and Lingering Fragility
When I was finally discharged, I felt stronger, though still fragile in ways that are hard to quantify. My body was improving, but my confidence lagged behind. I gathered my belongings slowly, folding hospital-issued clothing, packing toiletries, and checking drawers to make sure nothing was left behind. Before leaving, I stopped at the front desk. Gratitude had been building in me, and I wanted to express it properly. “I’d like to thank the nurse who checked on me every night,” I said. “The one assigned to my room.” The staff exchanged puzzled looks. One of them pulled up a schedule on the computer. Another flipped through printed assignments. They reviewed shift rotations and staffing records, double-checking carefully. After a few minutes, one of the women looked at me with a gentle expression that immediately made my stomach tighten. “There wasn’t a male nurse assigned to your room during your stay,” she said. “Only rotating female staff.”
When Reality Doesn’t Match Memory
They offered explanations kindly, without judgment. Stress, medication side effects, exhaustion. Sometimes patients perceive things differently during extended hospital stays, especially when pain management and disrupted sleep are involved. The mind, they explained, can fill in gaps as a coping mechanism. From a medical and psychological standpoint, it made sense. I nodded, accepted their explanation, and thanked them anyway. Yet as I walked toward the exit, a strange unease settled in my chest. Not fear exactly, but confusion mixed with reluctance to let go of something that had felt very real. Healing often brings moments we can’t fully explain, moments that don’t fit neatly into medical records or insurance justifications. I decided not to dwell on it. Recovery required focus, and I was eager to return home and rebuild my routine.
Returning Home With Questions Unanswered
At home, life resumed slowly. Familiar rooms felt slightly foreign at first, as if I were seeing them through a new lens. I followed follow-up instructions carefully, took prescribed medications on schedule, and kept appointments as recommended. Friends checked in more frequently now that I was out of the hospital. My children called when they could, relieved to hear strength returning to my voice. Outwardly, things improved. Internally, the memory of those quiet nights lingered. I found myself replaying them occasionally, wondering if I had misunderstood something, if fatigue had truly shaped my perception. The logical explanations were reasonable, even comforting. And yet, something about the consistency, the timing, and the words spoken each night didn’t feel random.
The Note I Wasn’t Expecting to Find
Weeks later, while unpacking a bag I had used during my hospital stay, I reached into one of the side pockets and felt something folded inside. It wasn’t a receipt or discharge paperwork. It was a small piece of paper, creased and worn, as if it had been folded and unfolded many times. I opened it slowly. Written in neat, deliberate handwriting were the words, “Don’t lose hope. You’re stronger than you think.” There was no name. No date. No hospital logo. No explanation. I sat down at the kitchen table and stared at the note for a long time. The room was quiet, but this time the silence didn’t feel oppressive. It felt reflective. My mind returned to those late evenings, the soft voice, the steady presence. Perhaps the note had been written by a staff member whose name I never learned. Perhaps it was written during a moment blurred by medication. Or perhaps it was something I was meant to find only after I had left that place behind.
What Comfort Really Looks Like
Whatever its origin, the note stayed with me. I placed it in a drawer at first, then later on my desk, where I could see it during difficult moments. It became a reminder that comfort doesn’t always arrive in ways we can document or explain. In a world driven by proof, records, and accountability, not every meaningful experience comes with a signature. Some of the most important support we receive leaves no trail, no invoice, no formal acknowledgment. It simply shows up when we need it most and leaves quietly, trusting that its impact will carry forward. That realization shifted something in me. I stopped needing to categorize the experience. I stopped asking whether it had a rational explanation or a symbolic one. What mattered was how it made me feel and what it helped me reclaim.
Strength That Emerges in Quiet Ways
Recovery taught me that strength isn’t always loud or dramatic. Sometimes it’s awakened by simple words spoken at exactly the right moment. Sometimes it’s reinforced by presence rather than action. During my hospital stay, my body healed through medicine, monitoring, and structured care plans designed to minimize risk and ensure compliance with health standards. But my spirit healed through something far less measurable. Feeling seen. Feeling encouraged. Feeling that someone, somewhere, believed I would make it through, even when I wasn’t sure myself. In the broader conversation about health, we often focus on treatments, costs, insurance coverage, and outcomes. Those things matter. They shape access and determine options. But experiences like this remind me that healing also happens in places beyond policy and procedure.
Carrying the Message Forward
I still don’t know exactly who wrote that note. I may never know. And I’ve learned that I don’t need to. The message itself was enough. It didn’t demand interpretation or explanation. It asked only that I receive it and carry it forward. In moments when fear creeps in or confidence falters, I remember those words. They’ve become part of how I approach challenges now, whether related to health decisions, financial uncertainty, or the quiet vulnerabilities that come with aging. Sometimes encouragement isn’t about who offers it. It’s about what it allows you to become afterward. And sometimes, that’s all you need to keep moving forward. There it is.